Saturday, March 19, 2022
Sunday, February 27, 2022
General Medicine E-Log
- Vesicular breath sounds heard
- Trachea is in central position
- No wheezing
- Dyspnoea is present
- Scaphoid shaped abdomen
- No tenderness
- No palpable mass, no organomegaly
- Bowel sounds are heard-sluggish
- Liver and spleen not palpable
- Drowsy and normal speech
- No neck stiffness
Thursday, October 28, 2021
CASE OF CHRONIC KIDNEY DISEASE
Sunday, October 24, 2021
GENERAL MEDICINE MONTHLY ASSIGNMENT
Evolution of symptoms were very well presented. Explanation for every treatment and causes were written in a very coherent manner.Overall it was very well explained and easy to understand.
CASE-2:
The history taking of the patient was written so orderly manner.As it has more pictures it was easier to understand the context.The important points were highlighted.The daily timeline routine helped in understanding the case in a better way.
CASE-3:
The case was very well presented and explained.All the keywords were highlighted which made it easier to get the concept and the mechanisms of treatment and the case were very well explained.The radiological information regarding the case made it easy to understand.The x-rays were made it better to understand.
CASE-4:
It has been elaborated in very good manner. The main points have been highlighted clearly.The pictures of investigation are posted in the elog which made it easier to follow up the case.The timely updates were also mentioned.The soap notes and plan of care was clearly mentioned.
CASE-5:
The explanation was good, but the certain points could have been highlighted. If a summary of patients details is given which made it much easier to understand.
CASE-6:
Very clean presentation and very well explained.It was easy to understand.Time line of treatment gave a huge help to understand the progression of patients situation.The pictures and x-rays and MRI scan pictures made it easy.
CASE-7:
The summary of the patient was mentioned which made it easier to understand.The presentation was neat, but certain points can be elaborated.The important words were highlited which made easier to understand the case.
CASE-8:
The patient history could have been elaborated to understand the case even more easily.The discharge summary was not given. Other than that everything is nicely presented.The scan reports were attached in orderly manner and time is mentioned regarding the investigation which is good.
CASE-9:
The patients case has been summarized it is easily understandable,the presentation was very neat and easy to understand.Main points were not highlighted.The time line events were posted with progress of patient's symptoms which is very well done.
CASE-10:
The case is presented well.The time line graph of vitals had helped to understand his progress clearly.Time line of laboratory investigations is give.This made me easy to understand whether he is reacting and getting better with the the medications given to him.
CASE-11:
The case was presented well.The summary at the end was a good idea it end with.The laboratory investigations well presented in coherent manner.
QUESTION-2,3:-
Please analyze the above linked long and short cases patient data by first preparing a problem list for each patient in order of perceived priority (based on the shared data) and then discuss the diagnostic and therapeutic uncertainty around solving those problems.
History of low grade fever, intermittent, not associated with chills and rigor.
Patient also complaints of yellowish discoloration of urine since 1 month, passing of clay colored stools since 1 month.
He also complaints of itching all over the body since 1 month, decreased appetite, loss of weight and generalised weakness since 1 month
Diagnostic approach and treatment
Antibiotic therapy (if indicated for infection)
- Endoscopic retrograde cholangiopancreatography (ERCP),
- Intravenous fluids and pain medications
(Captured by 2016 batch intern post final year mbbs) :
QUESTION-4:-
Testing competency in patient data capture and representation through ethical case reporting/case presentation with informed consent
Share the link to your own case report this month of a patient that you connected with and engaged while capturing his her sequential life events before and after the illness and clinical and investigational images along with your discussion of that case.
ANSWER-4:-http://uakanksha.blogspot.com/2021/10/case-of-chronic-kidney-disease.html
QUESTION-5:-
Tuesday, August 24, 2021
General Medicine Monthly Assessment
Evolution of symptoms were very well presented. Explanation for every treatment and causes were written in a very coherent manner.Overall it was very well explained and easy to understand.The history taking of the patient was written so orderly manner.It would have been better if more pictures were given directly which would make it easier to understand the context.
CASE-2:-
The case was very well presented and explained.All the keywords were highlighted which made it easier to get the concept and the mechanisms of treatment and the case were very well explained. It has been elaborated in very good manner. The main points have been highlighted clearly.If the pictures of investigation are posted in the elog it would be easier to follow up the case.The timely updates were also mentioned.
CASE-3:-
The explanation was good, but the certain points could have been highlighted. If a summary of patients details is given which made it much easier to understan.Very clean presentation and very well explained.It was easy to understand.Can add some more details about terapautic investigations.The summary of the patient was mentioned which made it easier to understand.The presentation was neat, but certain points can be elaborated.The links were attached from where the info was collected.The important words were highlited which made easier to understand the case.time line events were posted with progress of patient's symptoms which is very well done.
- Free water restriction for Hyponatremia
- Tab. PREDNISOLONE P/O 20 mg OD
- Tab FEBUXOSTAT P/O 80 mg OD
- Haemodialysis for worsening renal dysfunction
Ointment AMLORFINE
FUSIDICACIDCREAM
tabtelma 20 mg od .
TABHIZONE 15 mg per day in three divided doses @ 8am ,12 pm and 4 pm.
TabShelcal 500 OD and Tab Vit D 3 Od.
The patient history could have been elaborated to understand the case even more easily.The discharge summary was not given. Other than that everything is nicely presented.The scan reports were attached in orderly manner and time is mentioned regarding the investigation which is good.
Case-2:-
The patients case has been summarized it is easily understandable,the presentation was very neat and easy to understand.Main points were highlighted.The time line events were posted with progress of patient's symptoms which is very well done.Thecase is presented well.The time line graph of vitals had helped to understand his progress clearly.
Case-3:-
Time line of laboratory investigations is give.This made me easy to understand whether he is reacting and getting better with the the medications given to him.The case was presented well.The summary at the end was a good idea it end with.The laboratory investigations well presented in coherent manner.
Saturday, July 24, 2021
GENERAL MEDICINE-2
Evolution of symptoms were very well presented. Explanation for every treatment and causes were written in a very coherent manner.Overall it was very well explained and easy to understand.
CASE-2:
The history taking of the patient was written so orderly manner.It would have been better if more pictures were given directly which would make it easier to understand the context.
CASE-3:
The case was very well presented and explained.All the keywords were highlighted which made it easier to get the concept and the mechanisms of treatment and the case were very well explained.The histolgy information regarding the case made it easy to understand.
CASE-4:
It has been elaborated in very good manner. The main points have been highlighted clearly.The pictures of investigation are posted in the elog which made it easier to follow up the case.The timely updates were also mentioned.
CASE-5:
The explanation was good, but the certain points could have been highlighted. If a summary of patients details is given which made it much easier to understand.
CASE-6:
Very clean presentation and very well explained.It was easy to understand. Can add some more details about terapautic investigations.
CASE-7:
The summary of the patient was mentioned which made it easier to understand.The presentation was neat, but certain points can be elaborated.The links were attached from where the info was collected.The important words were highlited which made easier to understand the case.
CASE-8:
The patient history could have been elaborated to understand the case even more easily.The discharge summary was not given. Other than that everything is nicely presented.The scan reports were attached in orderly manner and time is mentioned regarding the investigation which is good.
CASE-9:
The patients case has been summarized it is easily understandable,the presentation was very neat and easy to understand.Main points were highlighted.The time line events were posted with progress of patient's symptoms which is very well done.
CASE-10:
The case is presented well.The time line graph of vitals had helped to understand his progress clearly.Time line of laboratory investigations is give.This made me easy to understand whether he is reacting and getting better with the the medications given to him.
CASE-11:
The case was presented well.The summary at the end was a good idea it end with.The laboratory investigations well presented in coherent manner.
QUESTION-4
Please analyze the above linked patient data by first preparing a problem list for each patient (based on the shared data) and then discuss the diagnostic and therapeutic uncertainty around solving those problems. Also include the review of literature around sensitivity and specificity of the diagnostic interventions mentioned and same around efficacy of the therapeutic interventions mentioned for each patient.
ANSWER-4
CASE-1:
Problem list:
•lower back ache
•burning micturition
•Fever with chills
•trauma to head
•mild hepatomegaly with grade 1 fatty liver
•high serum creatinine
•high blood urea
•pus cells in urine
Solution:
1)IVF : -RL @ UO+ 30ml/hr
-NS
2)SALT RESTRICTION < 2.4gm/day
3)INJ TAZAR 4.5gm IV/TID
2.25gm IV/ TID
4)INJ PANTOP 40mg IV/OD
5)INJ THIAMINE 1AMP IN 100ml NS IV/TID
6)INJ HAI S/C ACC TO SLIDING SCALE
8AM - 2PM - 8PM
7)SYP LACTULOSE 15ml PO/TID [ To maintain stools less than or equal to 2]
8) GRBS - 6th Hourly
9) BP/PR/TEMP - 4th Hourly
10) I/O - CHARTING
ON 10/7/21 :
1)IVF : -RL @ UO+ 30ml/hr
-NS
2)SALT RESTRICTION < 2.4gm/day
3)INJ TAZAR 2.25gm IV/ TID
4)INJ PANTOP 40mg IV/OD
5)INJ THIAMINE 1AMP IN 100ml NS IV/TID
6)TAB. PCM 500mg PO/ SOS
7)INJ HAI S/C ACC TO SLIDING SCALE
8AM - 2PM - 8PM
8)INFORM GRBS
9)GRBS - 6th Hourly
10) BP/PR/TEMP - 4th Hourly
11) I/O - CHARTING (STRICT)
12)T. ULTRACET PO 1/2 TAB QID
-Foley's removed,
13)INPUT UPTO 2 Liters only
CASE-2:
•lower back ache
•Dribble of urine
•Pedal edema
•High blood urea
•High serum creatinine
•Anemia
•Spondylodiscitis
•Tremours
Solution:
• Inj.Piptaz 2.25gm I.V -TID
• Inj.Lasix 40mg I.V -BD
• Inj.Pantop 40mg I.V -OD
• Nebulization budecort -8th hourly
• T.PCM 650mg -TID
• INJ. Neomol 1mg -I.V -SOS
• Temperature charting 4th hourly
• Monitor Bp,PR
• Left U/l elevation
• strict I/O charting
• Nebulization Salbutamol 2 repluses -6th hourly
• INJ. MAI 10u in 25% D over 45min I.V
15/7/21
• IVF -NS 0.9% &DNS U.O + 30ml/hr
• Inj. PIPTAZ 2.25gm -I.V -TID
• Inj.Lasix 40mg I.V -BD
• Inj.Pantop 40mg I.V -OD
• Nebulization Salbutamol 2 repluses -6th hourly
• T.PCM 650mg TID-after checking Temp.
• Temperature charting 4th hourly
• Monitor Bp,PR
• strict I/O charting
• Syp. Mucaine gel 10ml -BD
16/7/21
• IVF -NS 0.9% &DNS U.O + 30ml/hr
• Inj. PIPTAZ 2.25gm -I.V -TID
• Inj.Lasix 40mg I.V -BD
• Oral fluids upto 2-3liters/day
• Monitor Bp,PR ,Temperature
• strict I/O charting
• Limb elevation- Crepe bandage
• Syp.mucaine gel 15ml -TID
17/7/21
• Inj. PIPTAZ 2.25gm -I.V -TID
• Inj.Pantop 40mg I.V -OD
• Syp.mucaine gel 15ml -TID
• Limb elevation- Crepe bandage
• Monitor Bp,PR ,Temperature ,spo2%
• Tab.Febuxostat 40mg -OD
• Inj.Optinueron 1 ampule in 100ml NS /I.V/ OD
18/7/21
• Inj. PIPTAZ 2.25gm -I.V -TID
• Inj.Pantop 40mg I.V -OD
• Inj.Optinueron 1 ampule in 100ml NS /I.V/ OD
• Syp.mucaine gel 15ml -TID
• Limb elevation- Crepe bandage
• Monitor Bp,PR ,Temperature ,spo2%
• Tab.Febuxostat 40mg -OD
• Oral fluids upto 2-3L/day
19/7/21
• Inj. PIPTAZ 2.25gm -I.V -TID
• Inj.Pantop 40mg I.V -OD
• Inj.Optinueron 1 ampule in 100ml NS /I.V/ OD
• Syp.mucaine gel 15ml -TID
• Limb elevation- Crepe bandage
• Monitor Bp,PR ,Temperature ,spo2%
• Tab.Febuxostat 40mg -OD
• Oral fluids upto 2-3L/day
• Tab.Febuxostat 80mg -OD
• Tab.Neurobion forte -OD
• Syp.mucaine gel 15ml -TID
• Limb elevation- Crepe bandage
• Monitor Bp,PR ,Temperature ,spo2
• Oral fluids upto 2-3L/day
21/7/21
• Tab.Pantop 40mg -OD
• Tab.Febuxostat 80mg -OD
• Tab.Neurobion forte -OD
• Syp.mucaine gel 15ml -TID
• Limb elevation- Crepe bandage
• Monitor Bp,PR ,Temperature ,spo2
• Oral fluids upto 2-3L/day
• Inj.Ciprofloxacin 500mg-OD
22/7/21
• Inj. Ciprofloxacin 500mg-OD
• Tab.Febuxostat 40mg -OD
• Tab.Neurobion forte -OD
• Tab.pantop 40mg-OD
• Syp.mucaine gel 15ml -TID
• Limb elevation- Crepe bandage
• Monitor Bp,PR ,Temperature ,spo2
• Oral fluids upto 2-3L/day
- oral fluids upto 1.5 - 2 lit / day
- T. PAN 40mg /PO / OD
- T. ZOFER 4mg / PO /SOS
- TAB NODOSIS 550 mg / PO/BD
- Protein - x ( plant based ) 2 tablespoon in 1 glass of milk
- I/O charting
- BP / PR / Temp - 4th Hrly
- Neb c Duoun 2 respules 8th hrly
★11/7/2021
- oral fluids upto 1.5 - 2 lit / day
- Tab PAN-D PO/OD ( 8AM)
- T. ZOFER 4mg / PO /SOS
- TAB NODOSIS 550 mg / PO/BD
- Protein - x ( plant based ) 2 tablespoon in 1 glass of milk
- Inj ERYTHROPOIETIN 4000IVS/C weekly twice
- BP / PR / Temp - 4th Hrly
- T. OROFER - XT PO/BD
- Inj OPTINEORON 1 AMO IN 500ml NS IV/OD
- IVF -NS UO +30ml/hr
- RL
- I/O - CHARTING
★12/7/21
-inj.optineuron 1 amp in 500ml NS IV/OD
-ivf. NS RL @ uo + 30 ml/hr
-inj. erytropoitin 4000 iv s/c weekly twice
-tab.pan-d po/od (8 am)
-tab.orofer-xt PO/BD
-tab.nodosis 500mg PO/BD
-protein- x powder 2 tsp in 1 glass of milk PO/TID
-tab. zofer 4mg PO/sos
-BP/PR/Temp - 4th hrly
- I/o - charting
★13/7/2021
- Inj.optineuron 1 amp in 500ml NS SLOW/ IV/OD
-tab. pantop 40 mg RO/OD
-tab.nodosis 500mg PO/BD
-Protein- x powder 2 tsp in 1 glass of milk PO/TID
-I/o charting
- T.OROFER XT/OD
14/07/2021
- Inj.optineuron 1 amp in 500ml NS SLOW/ IV/OD
-tab. pantop 40 mg RO/OD
-tab.nodosis 500mg PO/BD
-Protein- x powder 2 tsp in 1 glass of milk PO/TID
-I/o charting
- T.OROFER XT/OD
2.TAB. NITROHART 20/37.5mg 1/2 T/D
3.TAB NICARDIA XL 30mg OD
4.TAB. GLICIAZIDE 80mg BD
5.TAB. NODOSIS 500 mg TD
6.Cap. BIO-D3 OD
7.Cap. GEMSOLINE OD
8.TAB. ECOSPRIN-AV 150/20mg OD
9.TAB.LASIX 40mg BD
10. SYP. LACTULOSE 15ml
- INJ THIAMINE 100 mg in 100 ml NS slow IV / TID
- INJ OPTINEURON 1AMP in 100 ml NS slow IV / OD
- INJ LASIX 40 mg
- TAB. ALDACTONE 50 mg PO / BD
- INJ PANTOP 40 mg IV/ OD
- ABDOMINAL GIRTH MEASUREMENT DAILY
- BP /PR/TEMP/ RR -4 hourly
- I/O CHARTHING
On 06/07/2021 :
1)PLENTY OF ORAL FLUIDS
2)INJ.METROGYL 400mg /IV/TID
3)INJ .CIPROFLOX 500mg /IV//OD
4)INJ.PANTOP 40mg iv/OD
5)INJ.THIAMINE 1amp in 100ml NS IV/TID
6)INJ.OPTINEURON 1ampin 100ml NS IV/od
7)TAB .SPORLAC DS PO/TID
8)ORS SACHET 1 in 1L OF WATER
9)TAB LOPERAMIDE. 2mg /po / SOS
10)BP/PR/TEMP/ RR 4 th hrly
11)I/O CHARTING.
On 07/07/2021 :
- PLENTY OF ORAL FLUIDS
- INJ.METROGYL 400mg /IV/TID
- INJ .CIPROFLOX 500mg /IV//OD
- INJ.PANTOP 40mg iv/OD
- INJ.THIAMINE 1amp in 100ml NS IV/TID
- INJ.OPTINEURON 1ampin 100ml NS IV/od
- TAB .SPORLAC DS PO/TID
- ORS SACHET 1 in 1L OF WATER
- TAB LOPERAMIDE. 2mg /po / Sos
- BP/PR/TEMP/ RR 4 th hrly
- I/O CHARTING.
On 08/07/2021
1)PLENTY OF ORAL FLUIDS
2)INJ.METROGYL 400mg /IV/TID
3)INJ .CIPROFLOX 500mg /IV//OD
4)INJ.PANTOP 40mg iv/OD
5)INJ.THIAMINE 1amp in 100ml NS IV/TID
6)INJ.OPTINEURON 1ampin 100ml NS IV/od
7)TAB .SPORLAC DS PO/TID
8)ORS SACHET 1 in 1L OF WATER
9)TAB LOPERAMIDE. 2mg /po / SOS
10)BP/PR/TEMP/ RR 4 th hrly
11)I/O CHARTING.
*12)TAB ECOSPIRIN 75mg/po/od
On 09/07/2021 :
1)PLENTY OF ORAL FLUIDS
2)INJ.METROGYL 400mg /IV/TID
3)INJ .CIPROFLOX 500mg /IV//OD
4)INJ.PANTOP 40mg iv/OD
5)INJ.THIAMINE 1amp in 100ml NS IV/TID
6)INJ.OPTINEURON 1ampin 100ml NS IV/od
*7)TAB LORAZEPAM 2mg OD
8)ORS SACHET 1 in 1L OF WATER
*9)TAB ECOSPORIN 75 mg OD
10)BP/PR/TEMP/ RR 4 th hrly
11)I/O CHARTING.
On 10/07/2021 :
1)PLENTY OF ORAL FLUIDS
2)TAB PANTOP 40mg iv/OD
3)INJ.THIAMINE 1amp in 100ml NS IV/TID
4)INJ.OPTINEURON 1ampin 100ml NS IV/od
5)TAB ECOSPORIN 75 mg OD
6)TAB LORAZEPAM 2mg OD
7)BP/PR/TEMP/ RR 4 th hrly
8)I/O CHARTING
On 11/07/2021 :
1)PLENTY OF ORAL FLUIDS
2)TAB PANTOP 40mg iv/OD
3)INJ.THIAMINE 1amp in 100ml NS IV/TID
*4)TAB NEUROBION FORTE OD
5)TAB ECOSPORIN 75 mg OD
6)TAB LORAZEPAM 2mg OD
6)BP/PR/TEMP/ RR 4 th hrly
7)I/O CHARTING.
On 12/07/2021
1)FLUID RESTRICTION <1.5L/ day
SALT RESTRICTION <2gm/day
2)Tab PAN 40mg iv/OD
*3)TAB. BENFOMETPLUS OD
*4)TAB NEUROBION FORTE OD
5)TAB ECOSPORIN 75 mg OD
*6)TAB LIVOGEN OD
*7)INJ. VITCOFOL 500mg IM/OD
*8)TAB. LASIX 20mg OD
*9)TAB. RIFAXIMINE 550mg BD
6)BP/PR/TEMP/ RR 4 th hrly
7)I/O CHARTING.
CASE-10:-
Problem list:-
•Pedal edema pitting type
•Fever
•Diabetes mellitus
•Acute kidney injury secondary to urosepsis
•Shortness of breath
•Increased serum creatinine
•Increased blood urea
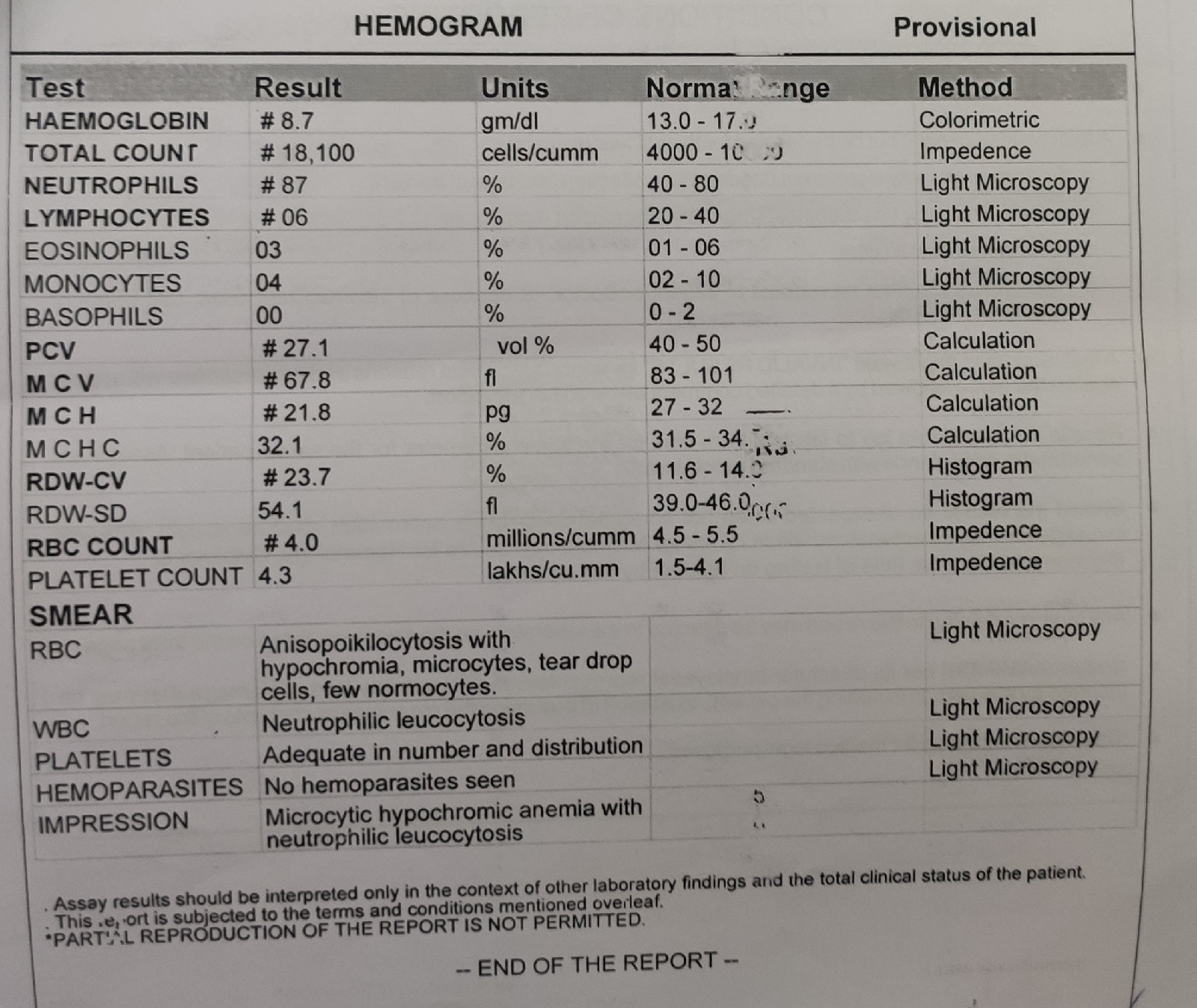
•Hemoglobin lower than normal
Solution:-
- Inj LASIX 40mg (8am- 2pm -8pm)
- IVF - NS @ UO + 50 ml/hr
- Inj LASIX 40 mg IV/TID 1 -1 - 1
- IVF - NS @ UO + 50 ml/hr
- Inj MAGNEXFORTE 1.5 gm/IV/BD
- Tab NODOSIS - XT PO/OD
- Inj HAI s/c
- Neb plain Asthalin 4 respules [ 1 - 1 - 1 - 1 ]
- Inj LASIX 40 mg IV/TID 1 -1 - 1
- IVF - NS @ UO + 50 ml/hr
- Inj MAGNEXFORTE 1.5 gm/IV/BD
- Tab NODOSIS - XT PO/OD
- Tab OROFEA - XT PO/OD
- Inj HAI s/c
- Neb plain Asthalin 2 respules
- Strict I/O charting
- Inj LASIX 40 mg IV/TID 1 -1 - 1
- IVF - NS @ UO + 50 ml/hr
- Inj MAGNEXFORTE 1.5 gm/IV/BD
- Tab NODOSIS - XT PO/OD
- Tab OROFEA - XT PO/OD
- Inj HAI s/c
- Neb plain Asthalin 2 respules QID
- Strict I/O charting
- Tab ULTRACET 1/2 tab QID [ 1/2 - 1/2 - 1/2 - 1/2 ]
- Inj LASIX 40 mg IV/TID 1 -1 - 1
- IVF - NS @ UO + 50 ml/hr
- Inj MAGNEXFORTE 1.5 gm/IV/BD
- Tab NODOSIS - 500 mg PO/OD
- Tab OROFEA - XT PO/OD
- Inj HAI s/c
- Neb plain Asthalin 2 respules QID
- Strict I/O charting
- Tab ULTRACET 1/2 tab QID[ 1/2 - 1/2 - 1/2 - 1/2 ]
- Inj LASIX 40 mg IV/TID [ 1 -1 - 1 ]
- IVF - NS @ UO + 50 ml/hr
- Inj MAGNEXFORTE 1.5 gm/IV/BD
- Tab NODOSIS - 500 mg PO/OD
- Tab OROFEA - XT PO/OD
- Inj HAI s/c
- Neb plain Asthalin 2 respules QID
- Strict I/O charting
- Tab ULTRACET 1/2 tab QID[ 1/2 - 1/2 - 1/2 - 1/2 ]
- BP/PR/SO2/Temperature monitoring
- GRBS charting
- Inj LASIX 40 mg IV/TID [ 1 -1 - 1 ]
- IVF - NS @ UO + 50 ml/hr
- Inj MAGNEXFORTE 1.5 gm/IV/BD
- Tab NODOSIS - 500 mg PO/OD
- Tab OROFEA - XT PO/OD
- Inj HAI s/c TID [ 10U - 8U - 8U ]
- Neb plain Asthalin 2 respules QID
- Tab Norflox 200 mg PO/BD
- Tab ULTRACET 1/2 tab QID[ 1/2 - 1/2 - 1/2 - 1/2 ]
- BP/PR/SO2/Temperature monitoring
- GRBS charting
- Strict I/O charting
- Inj LASIX 40 mg IV/TID [ 1 -1 - 1 ]
- IVF - NS @ UO + 50 ml/hr
- Tab Norflox 200 mg PO/BD
- Ing OPTINEURON 1amp in 100 ml NS IV/OD
- Tab OROFEA - XT PO/OD
- Tab SHELCAL-CT PO/OD
- Inj HAI s/c TID [ 10U - 8U - 8U ]
- Tab ULTRACET 1/2 tab QID[ 1/2 - 1/2 - 1/2 - 1/2 ]
- BP/PR/SO2/Temperature monitoring
- GRBS charting
- Strict I/O charting
- Inj LASIX 40 mg IV/TID [ 1 -1 - 1 ]
- Tab Norflox 200 mg PO/BD
- Tab ULTRACET 1/2 tab QID[ 1/2 - 1/2 - 1/2 - 1/2 ]
- Tab OROFEA - XT PO/OD
- Tab SHELCAL-CT PO/OD
- Inj HAI s/c TID [ 10U - 8U - 8U ]
- BP/PR/SO2/Temperature monitoring
- GRBS charting
- Strict I/O charting
QUESTION-5
osce and learning points - prefinals
OSCE- PREFINALS Case report:- https://uakanksha.blogspot.com/2023/12/a-65-yr-old-female-with-syncope.html Q. What is the best method to perf...
-
OSCE- PREFINALS Case report:- https://uakanksha.blogspot.com/2023/12/a-65-yr-old-female-with-syncope.html Q. What is the best method to perf...
-
CASE OF A 65 YEARS OLD FEMALE WITH SYNCOPE . This is an online e log book to discuss our patient's de-identified health data shared af...