135 U.Akanksha
Monday, December 4, 2023
osce and learning points - prefinals
Sunday, December 3, 2023
PREFINALS LONG CASE:-A 65 yr old female with syncope
CASE OF A 65 YEARS OLD FEMALE WITH SYNCOPE .
This is an online e log book to discuss our patient's de-identified health data shared after taking his/her/guardians' signed informed consent. This Elog reflects my patient-centered online learning portfolio.
This is the case of a 65 years old lady ,housewife resident of Chinatunalgudam.
The patient presented to the casualty after an episode of loss of consciousness .
Patient was apparently asymptomatic six days ago , when she had an episode of loss of consciousness , associated with sweating , and after walking for a long time .
Not associated with palpitation , flushing , chest pain , muscle weakness , slurring of speech, headache .
The patient was brought to the casualty and given medication and recovered completely .
6 days ago - History of chest pain ( sudden onset , in the centre of chest , squeezing type , non progressive , not radiating ) with shortness of breath following exertion , which were both relieved on rest .
She went to an RMP and was given an anti hypertensive agent .( which she consumed for the first time 3 days ago )
PAST HISTORY
No similar complaints in the past
She is a known case of hypertension since 3days
Not a known case of diabetes mellitus , asthma , tb , cerebrovascular accidents , coronary artery disease .
No blood transfusions .
History of treatment for cellulitis of leg .
FAMILY HISTORY
3 siblings with DM
PERSONAL HISTORY
Mixed diet , normal appetite
Adequate sleep
Normal bowel and bladder movements
No allergies
Addiction - sutta- 4 cigarettes/ day since 40 years
Alcohol or toddy - 1 glass daily
Daily routine
Wake up - 7 am
8 am - breakfast (rice )and tea
Afternoon (2:30pm)- lunch ( rice and curry )
Dinner - 9pm -rice and curry .
Sleep - 10 pm
GENERAL EXAMINATION
The patient is conscious , coherent and cooperative
Moderately built and moderately nourished
There is absence of Pallor , icterus cyanosis, koilonychia, lymphadenopathy .
Pedal edema present

VITALS
BP- 120/80mmHg in sitting position with cuff in the right hand at the level of the heart
PR- 67 bpm, normal rhythm ,
RR- 20cpm
Temp- Afebrile
SYSTEMIC EXAMINATION
CNS
Higher Mental Functions
Normal speech and language
Normal memory
No delusions or hallucinations
Cranial nerve examination
- I : Intact bilaterally
III, IV, VI : Extraocular movements free and full bilaterally
V : Intact bilaterally
VII:Intact bilaterally
VIII: No nystagmus, intact bilaterally
IX,X : Intact bilaterally
XII : Intact bilaterally
MOTOR SYSTEM
Bulk- normal
Power : normal power of
- Shoulder , Elbow , Wrist , Smalll muscle of hand and hand grip bilaterally
- knee , ankle bilaterally
Muscle tone :normal
Reflexes -normal : Biceps , triceps , knee jerk , ankle jerk bilaterally
Cerebellar signs : Normal
Sensory system examination
Upper limb : Normal
Lower limb
- Crude touch , temperature , fine touch ,vibration sensation present bilaterally
- Pain sensation is normal bilaterally
CVS
S1 S2 heard , no murmur
No thrill
Apical impulse felt
RESPIRATORY
Normal vesicular breath sounds in all areas
No adventitious breath sounds
PER ABDOMEN
Obese abdomen, umbilicus central and everted
Soft , non tender
No hepatomegaly no splenomegaly
PROVISIONAL DIAGNOSIS
?Syncope
?Hypotension
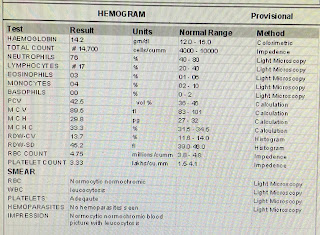
INVESTIGATIONS
Saturday, July 22, 2023
A 43 year old male with SEIZURES
Saturday, July 8, 2023
43 YEAR OLD MALE WITH SEIZURES
A 65 year old male with PAIN DISTENDED ABDOMEN and PAIN IN RT CHEST since 1 yr

osce and learning points - prefinals
OSCE- PREFINALS Case report:- https://uakanksha.blogspot.com/2023/12/a-65-yr-old-female-with-syncope.html Q. What is the best method to perf...
-
OSCE- PREFINALS Case report:- https://uakanksha.blogspot.com/2023/12/a-65-yr-old-female-with-syncope.html Q. What is the best method to perf...
-
CASE OF A 65 YEARS OLD FEMALE WITH SYNCOPE . This is an online e log book to discuss our patient's de-identified health data shared af...
-
Introduction: Welcome to my blog! I am U.AKANKSHA a 4th year medical student.This is an online E-log Entry Blog to discuss, understand and ...